Publications and research
Flawed research questions breastfeeding benefits
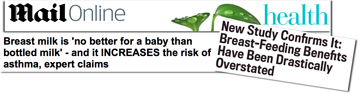
Research from Ohio University generated headlines around the world at the end of February by asking 'Is Breast Truly Best?' and suggesting not (the Daily Mail and Slate shown above). Our blog posting looking at the research more objectively received 10,000 visits the first weekend.
The research looked at a set of historic data and found that overall breastfed children did significantly better than formula-fed children. However, the researchers highlighted that in a subgroup no benefits were found from breastfeeding, comparing a child who may have only been breastfed once with a sibling who had no breastmilk at all. Professor Mary Renfrew told us this was one of the flaws: 'The exposure measures for breastfeeding were very crude. There was no measure of exclusivity, for example.'
Then out of 11 factors examined, 8 were to do with behavioural or scholastic outcomes at the ages of 4 to 14, such as their maths ability and vocabulary. Finding little difference between the subgroup children, they concluded that factors such as their parents' education have a bigger impact than how the children were fed.
The only health outcomes included in the research paper were body mass index (BMI), obesity and asthma. Drawing conclusions on the first two of these three is a difficult task in a country where over 35% of the population are classified as obese and nearly 70% have a BMI that classifies them as overweight or obese, particularly if one sibling may have been only partially breastfed. There is other evidence of less obesity in breastfed children and the Centre for Disease control suggests breastfeeding may help explain a recent fall in obesity rates (pg 24).
The NHS review of this research pointed out that in the subgroup of brothers and sisters fed differently there was actually no difference between reported asthma outcomes, from which you could conclude the feeding method does not have an impact on asthma risks if you follow the same logic the researchers use for reading and maths ability etc.
Not investigated was why did the mothers in the subgroup feed their children differently? The researchers simply say, 'all of the scenarios we can call to mind in which siblings are differently fed favor the breastfed sibling.' Really? How about: mother has a difficult breastfeeding experience that leaves her and her child distressed, so she switches to formula and then uses formula for her other children? That is all too common where breastfeeding support is lacking. There is no right to paid maternity leave in the US, so mothers are already facing severe obstacles when caring for young children.
Some have seized on the study to suggest that advocates should shut up about breastfeeding. However, the Breastfeeding Medicine blog pointed out the study authors drew a different conclusion:
If the secret ingredient is 'being born in a family where breastfeeding is possible,' then creating the conditions that enable families to breastfeed must be our highest priority. The take-away is that we need to fight for paid parental leave, high-quality childcare and a living wage for every family, regardless of how they decide to feed their infants.
• Colen, C.G., Ramey, D.M., Is Breast Truly Best? Estimating the Effects of Breastfeeding on Long-term Child Health and Wellbeing in the United States Using Sibling Comparisons, Social Science & Medicine (2014), doi: 10.1016/j.socscimed.2014.01.027.






